Minutes separated Are'Yana Hill from death as she struggled to breathe in the hallway of her San Francisco high school. The 18-year-old had lived with asthma attacks since before she could talk, and on that day, in April 2014, she could not speak. She thrust the rescue inhaler she carried in her backpack between her lips and inhaled. No relief. It felt, she thought, as if a charley horse had formed in her chest, knotting her lungs—each gasp trammeled by tightening airways. Her pursed lips turned gray, and all she could think about was her unborn baby. Hill, eight months pregnant, clutched her inhaler and prayed for paramedics to arrive.
"I take my medicine every day. I do everything the doctors tell me. I've tried every single thing, and I still have attacks," Hill said a little more than a year later, as a nurse at San Francisco General Hospital's Asthma Clinic placed a stethoscope on her back, between her shoulders. Her wheezing was barely audible. Each expiration sounded like the whistle of a distant tea kettle.
The attack in 2014 put Hill in the hospital. Asthma attack patients in the emergency room are often given oxygen and albuterol or other medications to relax the airways through a nebulizer mask. These treatments typically last a couple of hours, but Hill's airways weren't opening. She breathed through a nebulizer continuously for a week while the doctors closely monitored her pregnancy. Hill has brittle asthma—severe and unpredictable attacks that are poorly controlled, even with medication. Two weeks after she left the hospital, her son was born, healthy. Others are not as lucky.
Related: The Ugly Civil War in American Medicine
African-Americans, like Hill, are three times more likely to die of asthma than their white counterparts. Albuterol, the most commonly prescribed asthma medication in the world, is less effective in African-Americans and Puerto Ricans than in other racial and ethnic groups. According to one study, 47 percent of African-American kids and 67 percent of Puerto Rican kids with moderate to severe asthma didn't respond to albuterol; only 20 percent of Dutch kids with severe asthma weren't helped by the drug in a separate study . Blacks who use long-acting bronchodilators to control asthma are four times more likely to die or be hospitalized for severe asthma complications than whites.
It's not just about albuterol, and it's not just about asthma; genetic differences affect how minority groups respond to treatment for other diseases too. About 86 percent of Asian-Americans are estimated to have a genetic trait that makes them hypersensitive to warfarin, the most commonly used anticoagulant drug, putting them at risk of excessive bleeding at doses typically prescribed for white Americans. Only about 16 percent of white Americans have that trait. Up to 75 percent of Pacific Islanders have a genetic trait that makes them poor responders to the blood thinner clopidogrel, putting them at risk of recurrent heart attacks. Last year, in Hawaii, the state attorney general sued the makers of Plavix, claiming false, unfair and deceptive marketing, because the drug has little to no effect in an estimated 30 percent of the state's population.
What part of the world your ancestors came from can affect your disease risk and determine how your body metabolizes certain drugs. Yet 96 percent of participants in modern studies on disease genetics have been Caucasians, people of European descent. In the U.S., African-Americans and Hispanics make up nearly 30 percent of the population, yet account for only about 6 percent of all clinical trial participants. The result is a one-size-fits-all approach to medicine that benefits some segments of the population more than others. And the problem is bound to worsen: As the nation's interest and investment grow in precision medicine—medical therapies tailored to individual patients—the racial health disparity gap may be exacerbated if minority participants aren't better represented in future research initiatives, experts warn.
In a sunny hallway of Dr. Esteban Burchard's Mission Bay research laboratory hangs a framed print of Mexican artist Diego Rivera's "Flower Seller." In it, an indigenous Mexican woman kneels as she stretches to wrap her arms around a mighty bundle of calla lilies—Rivera's homage to the perennially downtrodden. "It reminds me why I come to work every day," he says.
Burchard, a pulmonologist at the University of California, San Francisco (UCSF), leads the nation's largest pediatric asthma research cohort composed entirely of blacks and Latinos. He has identified a genetic variant for severe asthma that is 40 percent more common in African-Americans than Caucasians. His research shows that ethnicity is the most important factor in determining whether a patient will respond to asthma therapy—even more important than the severity of the disease or the patient's socioeconomic status.
Like many of the participants in his study, Burchard grew up poor, just blocks from San Francisco General's Asthma Clinic, in the Mission District, a hotbed of Latin American political activism in the 1960s and 1970s. Half-Latino, half-Caucasian, Burchard and his four siblings were raised by their single Mexican-American mother, a schoolteacher. Chinese neighbors helped watch and feed him—he still speaks some Cantonese. Burchard was fascinated by the racial diversity he saw around him but frustrated by the rigid social structures girding it. "My mom was darker than me. Growing up, I could go places where she couldn't. I was so perplexed by that," says Burchard, who's made a career out of studying the nexus of genetic and socio-environmental factors that influence health and disease.
Related: Young Gay Men Aren't Getting the Health Care They Need
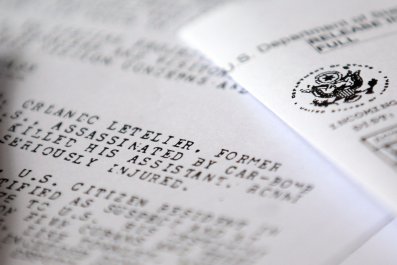
Historically, within medical research, African-Americans, Native Americans and other minorities were often relegated to unscientific experiments aimed at bolstering eugenics—such as the disfiguring procedures performed in the antebellum South by white physicians on non-consenting black slaves. In addition, they've historically been excluded from clinical and therapeutic trials that seek to uncover risk factors for disease and offer life-saving new treatments. Consider the infamous federally funded Tuskegee syphilis experiment—shut down in 1972—which denied treatment to hundreds of African-American men suffering from the disease.
In the U.S. medical community, studying racial differences in disease susceptibility and response to treatments remains controversial. Race and ethnicity are social constructs that have been used to marginalize and exploit. Scientifically, race serves only as a crude proxy for what experts call genetic ancestry—the diverse signatures that arose in the genetic code as our ancestors traversed the globe.

Some experts worry that a focus on finding genetic differences obscures the need to address the socioeconomic disparities that lead to uneven access to health care in the U.S. "Focusing on inclusion in clinical trials is a great way to ignore the fact that large numbers of poor and minority people are getting less than optimal health care," says Dr. Otis Brawley, chief medical officer for the American Cancer Society.
Yet because of its social baggage, race remains a powerful tool for studying patterns of disease and health, according to Sam Oh, an epidemiologist in Burchard's laboratory at UCSF. A person's self-identified race or ethnicity can offer important clues beyond genetic ancestry about important cultural, socioeconomic and environmental factors that may influence disease risk.
Nearly 30 percent of Dr. Latha Palaniappan's patients in the San Francisco Bay Area are of Asian descent. In the past, Asians were rarely included in clinical trials, says Palaniappan, an internist and medical researcher at the Stanford University School of Medicine. "For 1 out of every 3 patients I see, there is little research to guide my management. We are flying blind in terms of clinical care for Asian-Americans," she says. And when Asian-Americans are studied, says Palaniappan, researchers often focus on one Asian subgroup—leaving clinicians forced to extrapolate about disease risk and treatment for other Asian-Americans. This approach ignores the tremendous genetic and cultural diversity between different groups of Asian-Americans. Take heart disease. "If you lump all Asians together and compare them to the white population, heart disease risk looks about the same," says Palaniappan. "But if you look closer, you see that Chinese actually have a lower risk, while Asian Indians and Filipinos have a much higher risk."
Burchard made a similar discovery when he compared asthma rates among Latinos. Nearly 20 percent of all Puerto Ricans have asthma, while less than 5 percent of Mexican Americans suffer from the disease. He found that for Mexican-Americans, a higher percentage of Native American ancestry tended to be protective against asthma, while more African ancestry in Puerto Ricans predisposed many to asthma.
There are mechanisms to ensure racial equity in biomedical studies. The National Institutes of Health Revitalization Act, instituted by Congress in 1993, mandated inclusion of minorities in federally funded clinical research. But, says Moon Chen, an expert in cancer health disparities at the University of California, Davis, the act hasn't done its job. Last year, Chen and colleagues found that less than 2 percent of clinical cancer trials funded by the National Cancer Institute since 1993 focused on any racial or ethnic minority population. "The proportion of minority adults enrolled in cancer clinical trials is not adequate or representative of the U.S. population," they concluded. Total cancer incidence in minorities is expected to increase by 99 percent, compared with just 31 percent for whites, in the next 15 years. In addition, less than 5 percent of all lung disease studies funded by the National Institutes of Health (NIH) in the past two decades have included a statistically meaningful number of participants from racial or ethnic minorities, Burchard and colleagues reported earlier this year.
Primary investigators are mandated to submit an inclusion plan when applying for NIH-funded research, but there are few incentives to follow through. "We have not established any mechanisms of accountability or consequences for not doing it," says Dr. Eliseo Pérez-Stable, director of the National Institutes of Minority Health and Health Disparities, an NIH branch established through the Affordable Care Act to improve minority health and health disparities.
Studies show that minority researchers are more likely to focus their research on health disparities and addressing questions relevant to minority health. But minority physicians and scientists themselves are underrepresented among faculty at U.S. medical schools and research centers. They face additional barriers to getting their studies funded. For example, a 2011 review of grant applications to the NIH found that African-American and Asian-American researchers were 13 percent and 4 percent less likely to be funded than their white peers, respectively.
A dearth of minority researchers involved in grant review committees and other decision-making bodies can lead to subtle bias in the selection process, says John Dovidio, a psychologist at Yale University. "People tend to have more confidence in people like them. When you have to choose one applicant over the other, you're going to go with your gut. Racial bias colors that intuition in subtle ways," he says. In addition, practically, recruiting minorities into studies can prove challenging. Minorities are more likely to be poor and lack access to medical centers that refer patients for clinical studies. Cultural, linguistic and historical justice factors also create barriers.
In recent years, the NIH has taken steps to address problems with racial bias in the review process. It has funded investigations to understand how subtle bias occurs during the process and has taken steps to eliminate it, including launching a pilot program to make the review process anonymous. They've also funded initiatives to increase diversity in the biomedical workforce. Those efforts include partnering with universities to fund training and mentorship programs for minority students and young scientists pursuing careers in biomedical research.
While such steps may have a greater impact on the future generations of researchers, says Pérez-Stable, more needs to be done right now to incentivize the current field of research scientists and decision-makers to pay attention to the problem in a serious way. "The changing demographics of the U.S. make this an urgent issue, in my opinion," he says. More than half of all Americans will belong to a minority group by 2044, according to the U.S. Census Bureau. A growing number of taxpayers stand to be underrepresented in the medical research they help to fund, says Oh.
In January, President Barack Obama announced his Precision Medicine Initiative aimed at accelerating biomedical research on patient-centered treatments. The $215 million investment will include a research study of 1 million Americans. Kathy Hudson, deputy director for science, outreach and policy at the NIH, called recruitment of underrepresented minorities over the next two decades a "high priority" for the research initiative. The NIH has solicited feedback from doctors and scientists such as Burchard on how to create a diverse research cohort. The effort is an incredible opportunity to move forward on addressing questions of minority health, says Burchard, a member of the Precision Medicine Initiative Working Group, which has advised the NIH on how to recruit 1 million volunteers. "Getting it right is a matter of social and scientific justice."
This reporting project was funded through a grant provided by the Reporting Award at New York University's Arthur L. Carter Journalism Institute.